The Cost of Diabetes in Seven Graphs
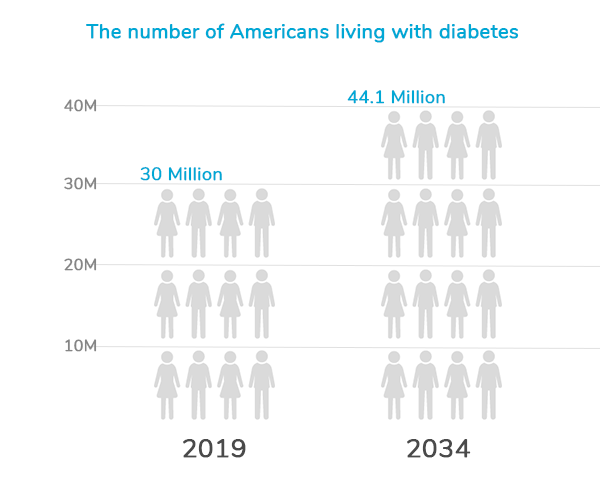
Diabetes is one of employers’ biggest concerns. Today, more than 30 million Americans live with diabetes, and it’s estimated the number will rise to 44.1 million by 2034. Largely sparked by a set of well-known risk behaviors – poor nutrition, physical inactivity, and tobacco use – diabetes is costly when left unaddressed. Improving health for those living with diabetes and preventing onset for those at-risk should be priority for all. At Premise, we believe there are seven charts that show why.
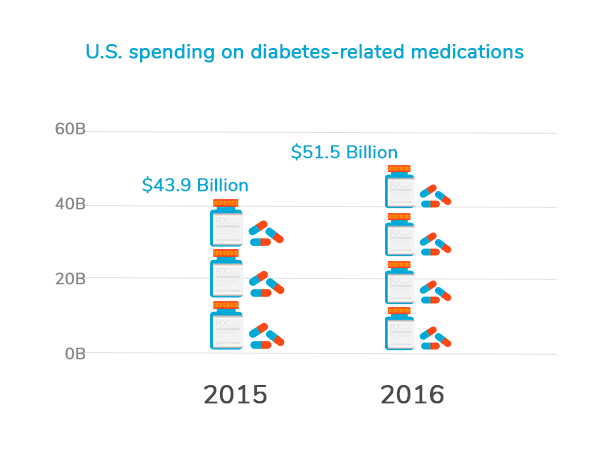
U.S. spending on diabetes-related medications increased from $43.9 billion to $51.5 billion from 2015 to 2016. One in 7 healthcare dollars is spent treating the condition and associated complications. As the U.S. healthcare system fights to address the rise of chronic conditions, employers are struggling to manage the costs their workforce accrues due to poor health.
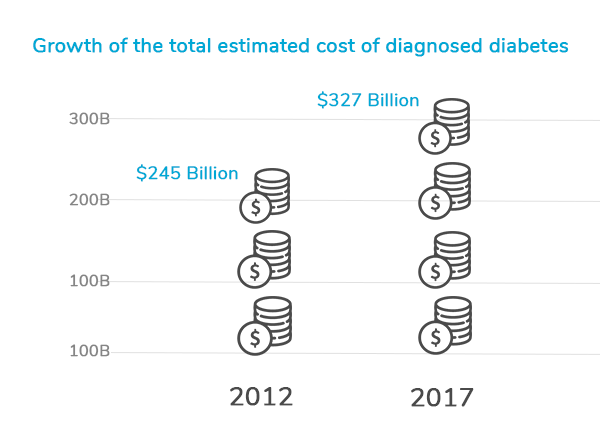
Costs – both direct and indirect – keep employers and their employees up at night. The total estimated cost of diagnosed diabetes has risen to $327 billion in 2017, up from $245 billion in 2012. This number accounts for direct medical expenses ($237 billion) and reduced productivity ($90 billion).
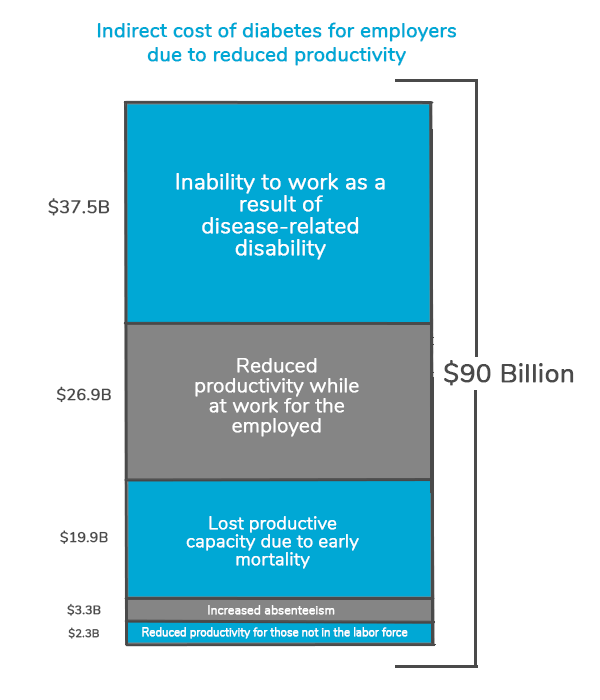
Employers indirectly take on a major part of this medical cost burden. Lost income due to missed workdays and reduced productivity create a costly snowball effect. According to a study by the American Diabetes Association, the $90 billion of reduced productivity can be broken down by the following:
- $3.3 billion: increased absenteeism
- $26.9 billion: reduced productivity while at work for the employed population,
- $2.3 billion reduced productivity for those not in the labor force
- $37.5 billion: inability to work as a result of disease-related disability
- $19.9 billion: lost productive capacity due to early mortality
Healthcare is one of
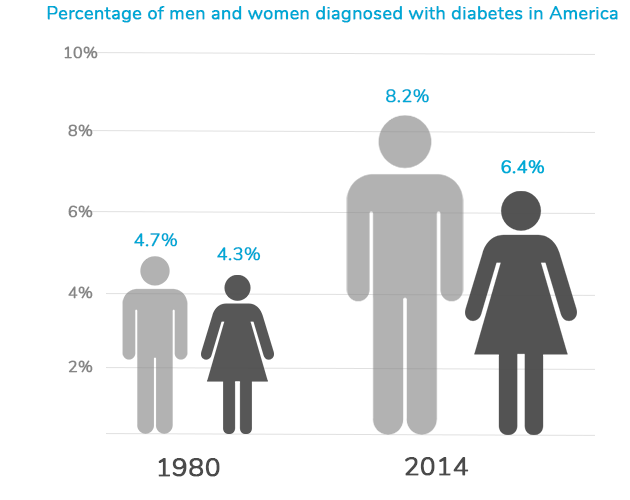
There is an obvious correlation between the increase in spending on treatment and the number of individuals living with diabetes. As the percentage of people with the condition increase, spending follows suit. Today, 9.4 percent of the U.S. population has diabetes
On average, people with diabetes pay 2.3 times more in medical expenditures compared to those without it. This is largely due to the costs of medication and doctors’ visits for correlated health issues, such as high blood pressure and unhealthy cholesterol levels. Chronic conditions are the lead reason people visit the doctor’s office, accounting for 37 percent of all encounters.
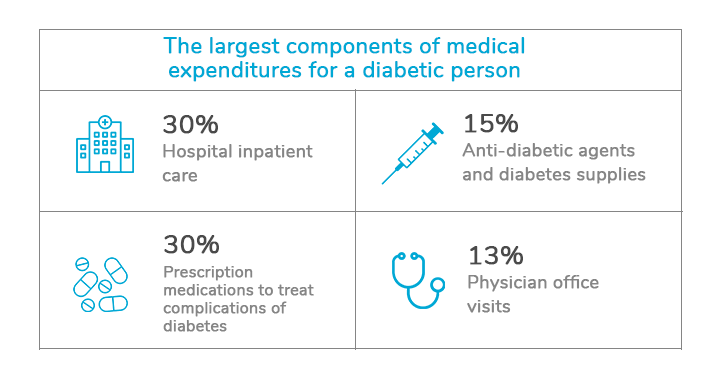
A recent report from the American Diabetes Association found the largest components of medical expenditures are:
- Hospital inpatient care (30% of the total medical cost)
- Prescription medications to treat complications of diabetes (30%)
- Anti-diabetic agents and diabetes supplies (15%)
- Physician office visits (13%)
If people don’t receive care when needed, or don’t follow their care plan, it can lead to costly, unnecessary care. Roughly 30 percent of emergency department visits among patients with common chronic conditions are potentially unnecessary, leading to $8.3 billion in additional costs for the industry, according to a new report. Unanticipated visits to an urgent care center or hospital can result in missed work days and lower productivity, ultimately impacting the employer’s bottom line.
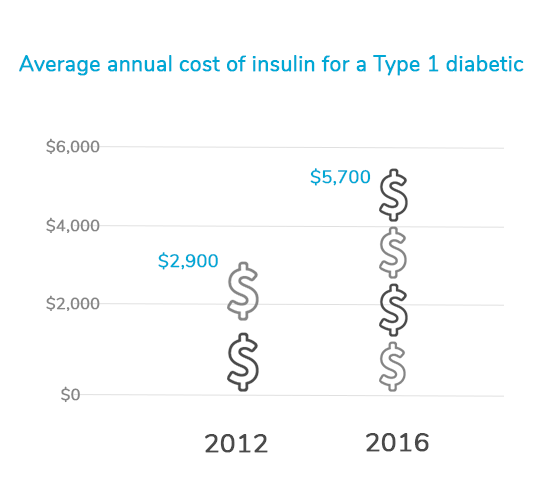
Medication adherence plays a large role in the health of a diabetic patient and the financial outcomes. In addition to making lifestyle changes, such as eating healthier and engaging in regular activity, many diabetic patients are on prescription drugs to help them manage the condition. The rising costs of managing diabetes can be attributed to significant increases in the cost of insulin. For people with Type 1 diabetes who use employer-sponsored health insurance, insulin spending per person increased 97 percent to $5,700 in 2016 from $2,900 in 2012. Insulin accounts for more than a third of the average annual cost for an individual managing diabetes, which is $18,500 on average, up from $12,500 in 2012.
As costs continue to rise, employers are in a unique position to take charge and drive positive outcomes. Organizations can play a role in improving the health of their populations by not only promoting healthy habits, but also bringing care directly to people to help them manage their conditions and create a culture of prevention.
Where Premise Health Fits In
Helping employers, their members and families change unhealthy behaviors and make better choices is foundational to our approach to care. Through an integrated model, we improve access to care, making it more convenient for members to get the care they need when they need it. Our provider teams get to know each member’s unique health situation, helping create personalized care plans to drive positive behavior changes. This approach leads to a better overall experience and delivers value for both the member – a healthier life – and organization – a healthy workforce and lower costs.
If you’re in charge of health at your organization, let us know how condition management affects your people. Get in touch – we value your questions and feedback.
Next on industry insights.
Healthcare Costs Are Employers’ Top Concern — Here’s How They’re Tackling Them
Read the Blog
How to Futureproof Your Healthcare Benefits
Read the Blog