Making BIG Pharma Feel Small(er) for Employers
As pharma costs continue to soar, employers are working to lessen the burden on their organizations and employees.
Today, Americans spend more on prescription drugs than anyone else in the world. On average, $1,100 comes out of every pocket each year. Specialty drugs are a big chunk. In the U.S., specialty drug spending is predicted to more than double by 2020, accounting for a significant portion of spending growth.
To help find ways to reduce drug costs, organizations have enlisted the help of pharmacy benefit managers (PBM) to negotiate rebates with drugs manufacturers and discounts from drugstores. But this tactic alone isn’t guaranteed to make a dent as specialty drug costs continue to soar.
Specialty drugs – the reason prescription drug spending is on the rise
Prescription drug spending is a significant contributor to overall healthcare spending. It’s also a pain point for employers and their employees; one in four people taking prescription drugs report difficulty affording their medication.
Due to the introduction of new, high-cost specialty drugs, the industry has seen an uptick in prescription drug spending in recent years:
- The introduction of specialty drugs for the treatment of complex, chronic, or rare conditions accounts for 36 percent of total drug spending.
- The largest proportion of new medicines launched in the last five years have been specialty drugs.
- Pharmaceutical spending grew 11.5 percent on a per capita basis in 2014, and 8.1 percent in 2015.
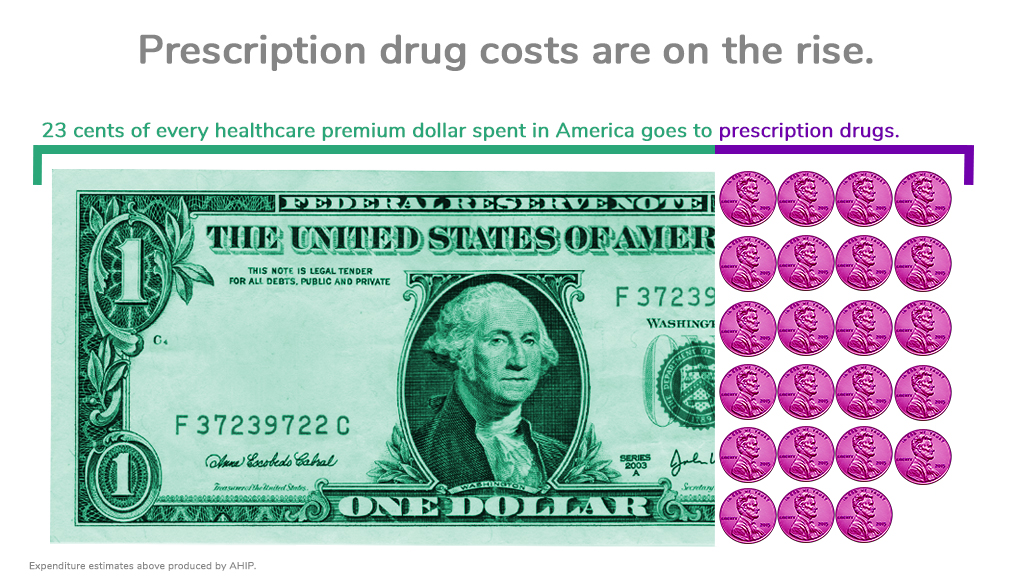
Unfortunately, patients are bearing the burden of these trends. Rising prescription drug costs account for more than 22 percent of every premium dollar, outpacing physician, inpatient, and outpatient hospital services, according to America’s Health Insurance Plans (AHIP). This equates to 23.3 cents of every
In addition, members pay roughly 17 percent of prescription medicine costs out of their own pockets. Organizations must take these stats into account as they evaluate their benefits strategy to reduce costs for themselves and their members.
To respond to rising specialty drug costs, employers should first consider their overall healthcare spend
Employers cite the high price of specialty drugs as the main driver behind escalating healthcare costs. Access to affordable options is also an issue, as these medications are considered “specialty” for a reason – they take years to develop and treat very specific conditions. Other options may not exist.
In response to specialty drug costs, many employers have adopted high deductible health plans, which share a greater portion of costs with employees. These plans may work for healthy employees, but they’re often not optimal for those with health conditions.
Other employers have contracted with mail-order pharmacy services that offer specialty drugs at discounted prices.
But these options aren’t always advantageous for the employer or its employees. To respond to rising specialty drug costs, employers first need to take a step back and look at their overall healthcare spend. Here are a few questions to consider:
- How do specialty drugs fit into the overall healthcare spend? While prescription drug costs are the highest spend for most employers, hospitalizations and other types of medical care typically aren’t far behind. It’s important to focus on strategies that help people be healthier overall, instead of strategies that only target drug costs.
- How much money am I saving through my PBM? PBMs offer invaluable services. But too often, organizations outsource their pharmacy benefits approach to a PBM without asking enough questions. It’s important to get the whole story to make informed decisions about benefit design.
- What is the benefit of using a mail order pharmacy? What are the drawbacks? Receiving medications in the mail is convenient. But it may not be the best choice for people who need specialty drugs. These medications can be difficult to administer or have strong side effects, which means it’s important for patients to interact with a pharmacist. Otherwise, they may not take the medication correctly, which can lead to complications –and higher costs.
There are no easy answers when it comes to benefit design, especially for specialty drugs. But it’s important to remember specialty drugs come with a higher price tag for a reason. If they provide a cure for a rare disease, they keep people out of expensive hospital settings and save costs in the long run. With a thoughtful approach, employers can make a difference in costs and help their people be healthier.

A different approach to pharmacy – The Premise Health model
As a direct healthcare company, we partner with organizations to bring pharmacy services to members at the workplace or in the community. Our pharmacists take an active role in members’ health, helping them know their options, understand their medications, and stick to them. It’s a seamless healthcare experience that creates value for clients and members.
See the onsite pharmacy in action. For a large manufacturer in South Carolina, our onsite pharmacy benefit resulted in an 87% medication adherence rate and a reduction of approximately $1,050 in healthcare expenses per enrolled member per year.
If you’re in charge of health at your organization, let us know how access to primary care affects your people. Get in touch– we value your questions and feedback.
Next on industry insights.

Why Payers Need Advanced Primary Care
Read the Blog
The Importance of Primary Care Access for Large Organizations
Read the Blog