How Primary Care Reduces Costs for Large Employers
Let’s face it: the traditional healthcare system doesn’t work. Rising medical costs and a shrinking provider workforce make it hard to see a doctor. In fact, nearly 1 in 3 Americans lack access to a primary care provider, according to a report from the National Association of Community Health Centers. This decrease in primary care utilization illustrates a major gap in our system. Not only does it lead to poor health outcomes for patients, but it also creates higher costs for employers.
If the traditional healthcare system doesn’t work, what does? Healthcare models like advanced primary care are designed to reduce costs for employers by improving access, integrating other types of care, and increasing primary care visits.
Great Experiences Lead to More Primary Care
Traditional healthcare isn’t known for its convenience. Long waits, short appointments, and large bills have led to patient burnout. But healthcare is different when employers and unions prioritize primary care. Direct healthcare models offer a patient-first approach and accessible primary care appointments through onsite or nearsite wellness centers. They also can connect patients to 24/7, on-demand virtual care. Meeting patients where they are so they can get the care they need, when they need it, makes it more likely a patient will make an appointment instead of delaying their care.
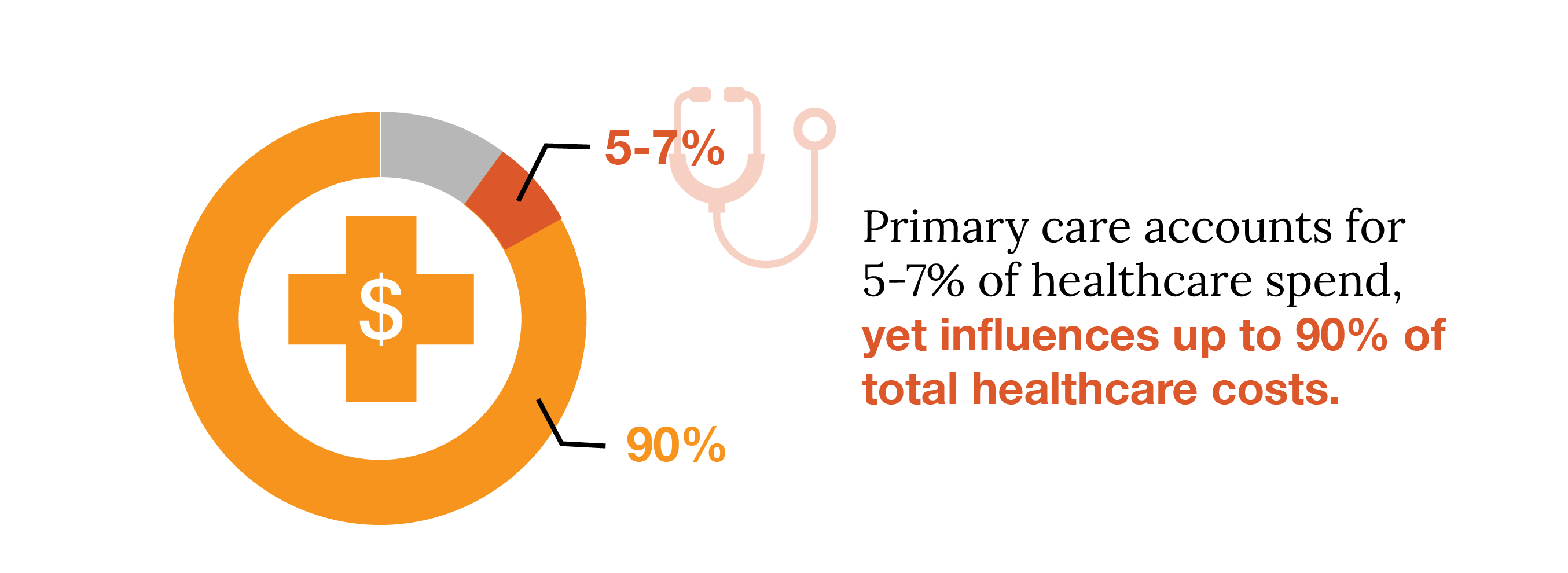
According to the Primary Care Collaborative, primary care accounts for 5-7% of healthcare spend, yet influences up to 90% of total healthcare costs. For employers, unions, and other self-funded organizations, making primary care easy-to-access means your people are getting more primary care for health issues they may have otherwise ignored, which drives down your total healthcare costs in the long run. Accessible care also means your employees or members are missing less work, so there are no disruptions to your business operations.
Integrated Advanced Primary Care Addresses Needs Early
Advanced primary care is an integrated healthcare model that brings together primary care, virtual care, behavioral health, pharmacy, Care Management, and Care Navigation. When your employees have access to multiple types of care all under one roof, there’s no longer a need to seek costly care in the community. A one-stop-shop means your people are receiving in-network care from a coordinated team that knows your benefits package. If specialty care is needed, a dedicated care navigator can recommend a high-quality, low-cost facility to avoid wasteful medical spend and duplicative care down the road. And with costly chronic conditions on the rise, having the support of a care manager helps your members stay on top of their medication and care plan, helping them get healthier, quicker – while avoiding costly trips to the hospital.
In an advanced primary care model, providers have access to data-driven insights that help them provide high-quality, cost-effective care. When they can see the full picture of members’ health, providers and analysts can help you address high healthcare costs by identifying your biggest areas of spend and high-cost, high-risk members. With this information, care teams are better equipped to educate members on where to go when they need care and help them avoid serious, disruptive medical events that carry significant health concerns and increase costs.
More Primary Care Means Less Emergency Care and Inpatient Admissions
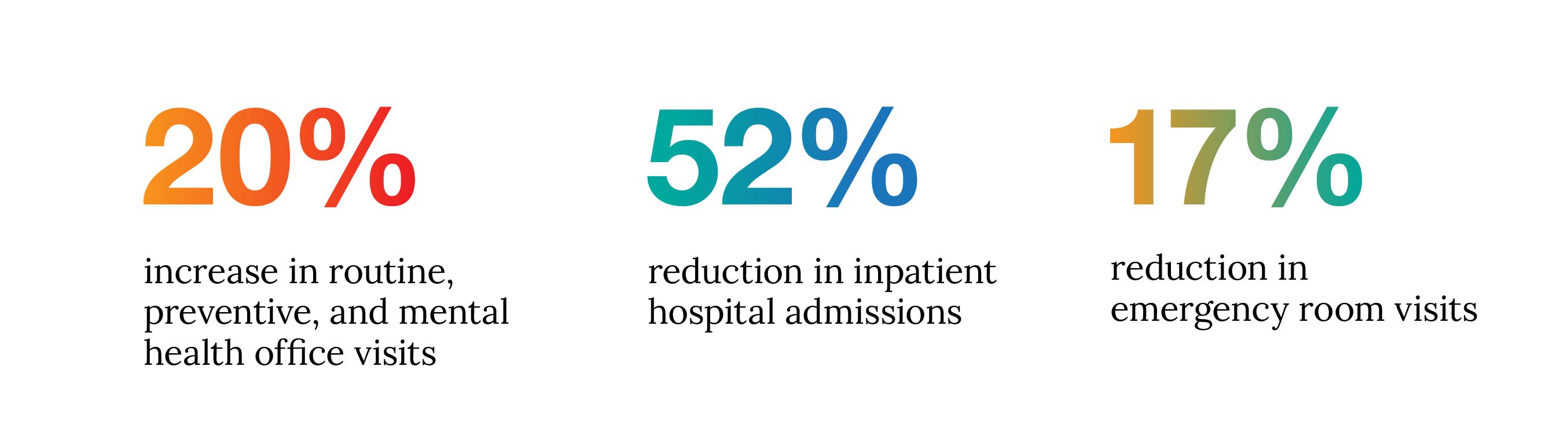
Studies show that primary care assists with the early management of health problems. Increasing the rate of preventive visits, and focusing on value over volume, helps decrease expensive downstream care needs like emergency room visits and hospital admissions. Primary care providers can also recommend relevant annual exams and screenings, which can further help their patients stay out of the hospital. This will ultimately impact your bottom line by avoiding expensive procedures and hospitalizations.
In a claims-based analysis of over 207,000 lives across 26 employers and unions, the data showed a 20% increase in the overall utilization of primary care, which led to a 52% reduction in inpatient hospital admissions and a 17% reduction in emergency room visits. It’s clear that easy access to primary care leads to better engagement, positive health outcomes, and higher cost savings for employers by addressing health issues early.
When people get more primary care, the healthcare system works better. At Premise Health, our advanced primary care model is healthcare working the way it should. Our recent industry-leading, claims-based analysis showed employers save an average of 30%, or $2,434, on the total cost of care for members and dependents attributed to a Premise onsite or nearsite wellness center, compared to those members and dependents who access care in their communities.
To learn more about how Premise’s advanced primary care model can positively impact your bottom line, contact us today.
Next on industry insights.

How to Futureproof Your Healthcare Benefits
Read the Blog
Why Partnering with an AAAHC Accredited Organization is a Win for Your Workforce
Read the Blog